Ultrasound in the Diagnosis of Prostate Cancer

Prostate cancer continues to be the second most common occurring cancer in men9. According to The American Cancer Society, the estimated number of new cases for 20211 are:
The good news is the survival rate is quite remarkable1: 98% at 5 years.
Prostate Cancer Diagnosis
Early detection is one of the most important factors in the successful treatment of any cancer. For the prostate, initial screening tools include:
- Prostate Specific Antigen (PSA) blood test: Elevation of PSA can be an early indication of prostate cancer2.
- Digital Rectal Examination (DRE): Nodules can often be palpated, as well as prostate enlargement, both of which can be early indicators of prostate cancer2
- Transrectal Ultrasound (TRUS) of the prostate: Ultrasound is used to identify suspicious nodules within the prostate. TRUS is also used to calculate prostate volume. Nodules and prostate volume enlargement can be early indicators of prostate cancer2.
- Transrectal Ultrasound Guided Biopsy: Once the suspicion of prostate cancer is elevated enough, the next step is usually a biopsy. Currently, a 12-core biopsy of the prostate is the common approach2. However, MRI/ultrasound fusion biopsy is rapidly gaining popularity3.
While prostate sonography has been around for more than 4 decades, it is currently undergoing a bit of a renaissance. This resurgence can be attributed to several factors, primarily the ongoing improvements and utilization of:
- Prostate MRI/ultrasound fusion imaging and biopsy
- Prostate contrast imaging and biopsy
Prostate MRI/ultrasound Fusion Imaging and Biopsy
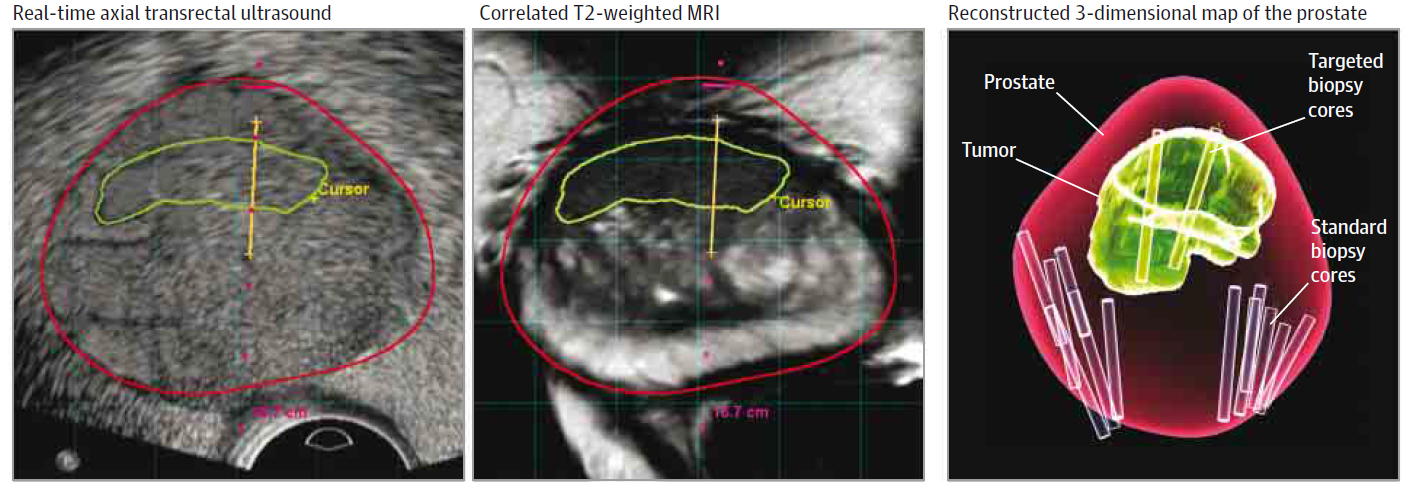
Prostate MRI/ultrasound fusion imaging and biopsy are powerful advancements in the visualization and subsequent biopsy of suspicious prostate nodules and biopsy guidance. Historically, transrectal ultrasound (TRUS) of the prostate has not been as accurate at identifying suspicious nodules within the prostate as MRI3,4.
According to a recent online article by the Journal of American Medical Association (JAMA):
MRI/ultrasound fusion biopsy can be performed using a transrectal or transperineal approach using a CIVCO endocavity balloon for accurate prostate positioning and a CIVCO Micro-Touch™ Stabilizer with the Classic or EX3™ Stepper.

Prostate Contrast Imaging and Biopsy
Contrast-enhanced ultrasound (CEUS) may improve the visualization of the prostate and better detect specific areas of cancer. CEUS uses intravenous contrast to better visualize areas of increased blood flow within the prostate, which may be indicative of latent prostate cancer.
Global research has produced numerous studies demonstrating improved prostate cancer detection with the use of contrast-enhanced ultrasound biopsy techniques. Vascular areas visualized and targeted for biopsy using these techniques yield improved cancer detection rates.
Targeted biopsies using CEUS of the prostate have a higher yield for prostate cancer detection and may prove useful for the initial evaluation of patients with elevated PSA6.
Prostate sonography has been around for over four decades, but its popularity is increasing with the advent of new technologies such as fusion, contrast-enhanced imaging, and the increased use of hydrogel.
You can find additional information on the referenced and all CIVCO products at www.CIVCO.com.
References
- American Cancer Society, "Prostate Cancer Statistics, 2021," https://cancerstatisticscenter.cancer.org/#!/cancer-site/Prostate
- Guidelines for the management of clinically localized prostate cancer. American Urological Association 2007, Reviewed and accepted 2011
- Ahmed H, Bosaily A, Brown L, Gabe R, Kaplan R, Parmar M, Collaco-Moraes Y , Ward K, Hindley R, Freeman A, Kirkham A, Oldroyd R, Parker C, Emberton M, and the PROMIS study group "Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study" Lancet. 2017 Feb 25;389(10071):815-822.
- M Siddiqui, S Rais-Bahrami, B Turkbey, et al; "Comparison of MR/Ultrasound Fusion–Guided Biopsy with Ultrasound-Guided Biopsy for the Diagnosis of Prostate Cancer" JAMA. 2015;313(4):390-397. doi:10.1001/jama.2014.17942
- admetech.org/researchers-look-to-mri-and-biomarkers-to-help-improve-detection-of-aggressive-prostate-cancers/
- Kundavaram C, Halpern E, Trabulsi E "Value of contrast-enhanced ultrasonography in prostate cancer" Curr Opin Urol.2012 Jul;22(4):303-9
- Hamstra D, et al. Continued Benefit to Rectal Separation for Prostate RT: Final Results of a Phase III Trial. Int J Radiat Oncol Biol Phys; Dec. 2016 DOI
- Hamstra D, et al. Evaluation of sexual function on a randomized trial of a prostate rectal spacer. J Clin Oncol 35, 2017 (suppl 6S; abstract 69)
- World Cancer Research Fund & American Institute for Cancer Research, "Worldwide cancer data," 2018, https://www.wcrf.org/dietandcancer/worldwide-cancer-data/












